What Affects Blood Supply Of Lower Leg? Improve Circulation
The intricate network of blood vessels responsible for supplying oxygen and nutrients to the lower leg is a complex system that can be influenced by a multitude of factors. Understanding these factors is crucial for maintaining healthy circulation and preventing conditions that can lead to reduced blood flow. The lower leg, comprising the calf, ankle, and foot, relies on a robust blood supply to function properly, especially during physical activities. Any compromise in this supply can lead to discomfort, pain, and potentially severe complications.
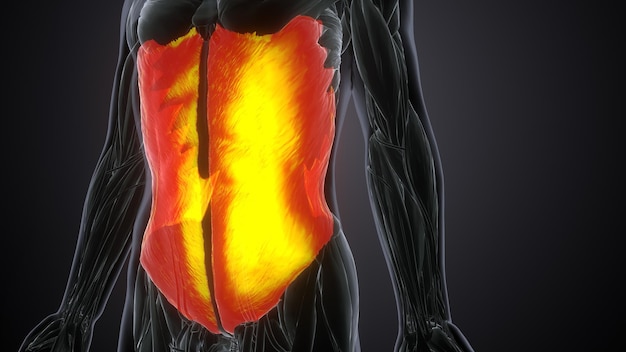
Anatomy of Lower Leg Blood Supply
Before delving into the factors that affect blood supply, it’s essential to grasp the basic anatomy involved. The primary arteries responsible for the blood supply to the lower leg include the popliteal artery, which branches off into the anterior and posterior tibial arteries. These arteries further divide into smaller branches that reach the muscles and tissues of the lower leg. The venous system, comprising superficial and deep veins, returns deoxygenated blood back to the heart. This intricate vascular network is susceptible to various influences that can either enhance or impede its function.
Factors Affecting Blood Supply
Several factors can impact the blood supply to the lower leg, ranging from lifestyle choices to underlying medical conditions. Understanding these factors can help in adopting preventive measures or seeking appropriate medical intervention.
Smoking: One of the most significant risk factors for reduced blood flow is smoking. Chemicals in tobacco can damage the lining of blood vessels, leading to narrowing and hardening of the arteries (arteriosclerosis), which severely restricts blood flow.
Diabetes: High blood sugar levels over time can damage blood vessels and nerves, affecting circulation. Diabetic patients are at a higher risk of developing peripheral artery disease (PAD), which reduces blood flow to the limbs.
Physical Inactivity: Leading a sedentary lifestyle can contribute to poor circulation. Regular physical activity helps strengthen the heart and improves the efficiency of the vascular system, ensuring better blood flow to all parts of the body, including the lower leg.
Obesity: Excess weight can put additional strain on the vascular system, increasing the risk of developing conditions like varicose veins and deep vein thrombosis, which can affect blood circulation.
High Blood Pressure: Uncontrolled hypertension can cause blood vessels to become overstretched and damaged, leading to decreased elasticity and efficiency in blood flow regulation.
Age: As people age, the risks of vascular diseases increase, partly due to the accumulation of plaque in arteries over time, which can narrow the arteries and reduce blood flow.
Family History: Genetic predisposition can play a role in the development of circulatory diseases. Individuals with a family history of vascular conditions should be particularly vigilant about maintaining a healthy lifestyle.
Diet: A diet high in saturated fats, cholesterol, and sodium can contribute to the development of atherosclerosis, affecting blood vessel health and, consequently, circulation.
Improving Circulation
Fortunately, there are several strategies to improve circulation to the lower leg, many of which involve lifestyle modifications.
Regular Exercise: Engaging in physical activities like walking, cycling, or swimming can significantly enhance blood flow. Exercises that target the calf muscles, such as toe raises and calf presses, are particularly beneficial.
Healthy Diet: Adopting a diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain vascular health. Foods high in omega-3 fatty acids, such as fish, and antioxidants, found in berries and leafy greens, are especially beneficial.
Smoking Cessation: Quitting smoking can immediately begin to improve vascular health and circulation.
Stress Management: Chronic stress can have a negative impact on circulation. Engaging in stress-reducing activities like yoga, meditation, or deep breathing exercises can help mitigate this effect.
Elevation and Movement: For individuals who spend a lot of time sitting or standing, regularly elevating the legs above the level of the heart and taking short walks can help improve venous return and reduce swelling.
Compression Stockings: Wearing compression stockings can be beneficial for individuals with venous insufficiency or those at risk of developing deep vein thrombosis, as they help improve blood flow back to the heart.
Conclusion
Maintaining a healthy blood supply to the lower leg is crucial for overall well-being and mobility. By understanding the factors that can affect circulation and adopting strategies to improve vascular health, individuals can reduce their risk of developing circulatory diseases. A combination of lifestyle modifications, awareness of risk factors, and, when necessary, medical intervention can ensure that the blood supply to the lower leg remains robust and efficient, supporting an active and healthy lifestyle.
What are the symptoms of poor circulation in the lower leg?
+Symptoms can include pain or cramping in the legs, numbness or tingling, coldness or discoloration of the skin, and slow healing of wounds. If you experience any of these symptoms, it's essential to consult with a healthcare professional.
How can regular exercise improve circulation in the lower leg?
+Exercise helps strengthen the heart, improving its efficiency in pumping blood. It also enhances the flexibility and elasticity of blood vessels, allowing them to dilate and constrict more effectively, thus improving blood flow to the lower leg.
What role does diet play in maintaining healthy circulation?
+A healthy diet rich in fruits, vegetables, whole grains, and lean proteins supports vascular health. Foods high in antioxidants and omega-3 fatty acids are particularly beneficial, as they help reduce inflammation and improve the health of blood vessels.
In conclusion, while several factors can affect the blood supply to the lower leg, a proactive approach that includes lifestyle modifications, awareness of risk factors, and timely medical intervention can significantly improve circulation and reduce the risk of associated diseases. Adopting these strategies can lead to a healthier, more active life, where mobility and comfort are not compromised by poor circulation.